Home > Highlighting JAPAN > Highlighting Japan DECEMBER 2011 > New Nose Cartilage Treatment at Clinical Study Stage
Highlighting JAPAN
SCIENCE
New Nose Cartilage Treatment at Clinical Study Stage
Human cartilage is indispensable for retaining the shape of the nose and ears and for facilitating joint movement. When cartilage acquires a defect or deformation due to illness, injury or congenital abnormality, however, it is nearly impossible for it to heal naturally. This serious consequence that patients encounter is about to gain a ray of hope in implant-type tissue-engineered cartilage. Takashi Sasaki interviewed two of the specialists involved in this development, Tsuyoshi Takato and Kazuto Hoshi.
Implant-type Tissue-engineered Cartilage
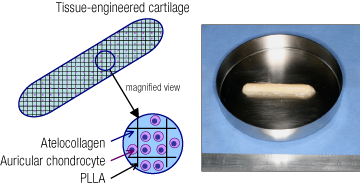
Implant-type tissue-engineered cartilage sample (photo). The cartilage is formed by auricular chondrocytes and a scaffold made of poly-L-lactic acid (PLLA) and atelocollagen.
"Unlike bone, cartilage has poor self-repairing ability and there is very limited availability of cartilage extractable from other areas of the patient's body. This is why studies for tissue-engineered cartilage have been conducted around the world by culturing and increasing chondrocytes," says Professor Takato, who is responsible for treating patients. "However, the currently available tissue-engineered cartilage is in a gel or liquid form and cannot be hardened or formed so that it is suitable for treatment of the ears or nose."
In the past, implanting bone, rather than cartilage, was one of the common methods for treating patients with deformed nasal cartilage resulting from cleft lip palate or the like. The shortcoming of inflexible bone was susceptibility to fracture even with a small impact. Patients with this symptom reportedly struggled against numerous difficulties in such everyday activities as wearing glasses and blowing the nose.
To address these difficulties, Associate Professor Hoshi took the lead in development of tissue-engineered cartilage that is approximately 50 mm long, 6 mm wide and 3 mm thick. This is a design exclusively for nasal treatment. The new type of tissue-engineered cartilage is made by including extracorporeally cultured chondrocytes into the scaffold made of specialized plastic and collagen, and can be safely absorbed in vivo. This is called an "implant-type" method since it involves surgically implanting the cartilage into the body.

Tsuyoshi Takato (right) and Kazuto Hoshi, respectively professor and associate professor at the University of Tokyo Hospital.
The treatment method developed by Professor Takato and his group is now in the clinical study stage. One patient who underwent surgery for implanting the tissue-engineered cartilage into the nose is reportedly in good condition. After transplantation, the chondrocytes begin to produce the substances specific for cartilage within the scaffold that mechanically protects the chondrocytes and gradually regain the properties of the original cartilage. As a result, the cartilage almost completely recovers both in terms of appearance and functionality. After that, the scaffold remaining in the affected area is slowly absorbed. Years later, only the cartilage of the patient is rooted in the affected area.
"Organ transplantation may involve the use of an organ from another person or animal, or an artificial organ," Professor Takato says, as he explains the prospects of the implant-type tissue-engineered cartilage. "This inevitably entails the risk of a rejection reaction or exposure to unknown pathogens. Implanted with the use of the cells harvested from the patient, the tissue-engineered cartilage has a high level of safety and a substantial advantage in that it easily assimilates into the body. Treatment thus far has focused on the nose and ears. Continued efforts for development will even make it possible to treat complexly formed areas such as the trachea. Our goal is its application to heavily loaded cartilage, such as joint cartilage. This will lead to competition against artificial joints that have already been put into practical application."
The group led by Professor Takato is continuing its clinical studies, aiming for commercialization in five years. Their efforts are drawing a great deal of attention in the field of regenerative medicine, where researchers around the world engage in heated competition.
© 2009 Cabinet Office, Government of Japan






